
Welcome to Amanda's NICU Education




Hi! My name is Amanda. I'm a NICU nurse, Clinical Nurse Specialist, NICU Educator... basically your NICU BFF. If you want to talk NICU, I'm here for you! I love everything about NICU nursing and I'm eager to learn and share my knowledge with all my NICU friends.
I have been a NICU nurse since 2009 I am currently a Clinical Nurse Specialist in a Level IV NICU in Los Angeles.
I am passionate about educating the next generation of NICU nurses. I share my knowledge through platforms such as Instagram and Facebook and am excited to have you here on my website!
Click on the button below to sign up for my newsletter filled with NICU education and tips for all experience levels.

Not very many people love taking tests but as a self-acclaimed "forever student" who has taken (and passed) five different certification exams I am no longer afraid of tests! "Way to brag", you might be thinking but I want to help YOU pass your certification exam too!
Introducing Amanda's RNC-NIC Success digital course - your ultimate study companion!
Gain unlimited, on-demand access for life, ensuring you're primed to ace your certification exam.
I'm here to help you succeed and I can't wait for you to share with me that you PASSED the RNC-NIC EXAM!!!









Congenital Infections
Neonatal Congenital Infections
Congenital infections are a major concern for neonatal health, often leading to a range of complications. Oftentimes, these infections are characterized by the acronym TORCH, standing for toxoplasmosis, other (syphilis, enterovirus, parvovirus, etc.), Rubella, CMV, Herpes Simplex (HIV, and Hepatitis). Prenatal screening for congenital infections are generally performed in the first trimester.
Here's a review of common congenital infections that you will definitely need to know!

Toxoplasmosis
Toxoplasmosis is caused by the protozoan parasite “Toxoplasma gondii”. Mothers can acquire the infection from undercooked meat, unwashed fruits and vegetables or contact with infected cat feces. The highest risk occurs when a mother has a primary acute infection during pregnancy. While 60-80% of affected newborns show no symptoms, some (less than 10% of cases) may have the classic triad of chorioretinitis, hydrocephalus, and intracranial calcifications. Chorioretinitis is the most common late finding.
Congenital toxoplasmosis is diagnosed via PCR or observation of the parasite in tissues. Treatment involves a 3-12 month regimen of pyrimethamine, sulfadiazine, and folinic acid, often combined with glucocorticoids if vision is threatened. Additionally, ophthalmologic exams every 3-6 months during the first 3 years of life and neurodevelopmental follow up is necessary for babies diagnosed with congenital toxoplasmosis.

Mcleod et al, 2014
Rubella
Congenital rubella syndrome can cause severe birth defects, including hearing loss, cataracts, heart defects, and intellectual disabilities. Some babies present with a blueberry muffin rash at birth. Though rare in the U.S. due to immunization efforts, rubella remains endemic in other regions. Diagnosis involves detecting rubella-specific IgM antibodies or rising IgG titers in newborns. While there is no specific treatment, prevention through maternal vaccination before pregnancy is crucial. Pregnant women and newborns with proven or suspected rubella should be cared for under isolation precautions.

Example of a Blueberry Muffin Rash
New England Journal of Medicine
Cytomegalovirus (CMV)
CMV is the most common congenital viral infection (I would know that for the certification exam) and is transmitted through blood and bodily fluids. Although many infected infants are asymptomatic, some may develop complications such as hearing loss, developmental delays, and seizures. Some signs of CMV include low birth weight, jaundice, microcephaly, and hepatosplenomegaly. Hearing loss occurs in up to 50% of symptomatic infants and up to 15% of asymptomatic infants, therefore repeated auditory exams are recommended during the first 6 years of life.
Diagnosis is confirmed through viral isolation in urine or saliva and high anti-CMV IgM titers within the first 3 weeks of life. Treatment typically involves the antiviral agents ganciclovir or valganciclovir, which can help reduce hearing loss and developmental delays.
While CMV can be transmitted through breast milk, it is generally not contraindicated for breastfeeding in term babies. NICU nurses should be mindful that CMV infections can be transmitted to vulnerable premature infants via breast milk resulting in a sepsis-like illness. Freezing breast milk can reduce replication of CMV, however feeding fresh breastmilk has benefits for the gut microbiome that can reduce the risk of NEC. The decision whether to freeze breast milk prior to administering should consider the risks for each individual infant.
Check out this great video on congenital CMV
Herpes Simplex Virus (HSV)
Neonatal HSV can result in serious complications, especially if it disseminates to multiple organs. HSV is transmitted during birth from an infected genital tract or, less commonly, postnatally through contact. Mothers with active genital lesions are delivered by cesarean sections to prevent HSV transmission. Signs of HSV infection may include vesicular lesions, seizures, and septic shock. HSV infections are categorized as a localized “Skin Eye Mouth (SEM)” disease, “Disseminated disease” or “Localized CNS” disease. Localized SEM is most common (about 45% of cases) and typically presents around 7-14 days of life. Disseminated disease affects about 25% of cases and also presents at 7-14 days of life with severe liver dysfunction, abnormal CSF findings, seizures, profound sepsis, and septic shock. Localized CNS disease affects about 30% of cases and typically presents around 14-21 days of life. Diagnosis is confirmed by viral culture from vesicular fluid or CSF. Treatment involves acyclovir for up to 21 days, with suppressive therapy continuing for 6 months to improve neurodevelopmental outcomes.

Sánchez et al, 2022
Enterovirus
Enteroviruses, often spread through the fecal-oral and respiratory route, can cause severe neonatal infections, especially during the summer and early fall (June-October). There are many types of enteroviruses (coxsackie virus, echovirus, etc.) and they are commonly transmitted around the time of delivery. For most adults and children enterovirus infections are mild, however in neonates these viruses can lead to multiorgan dysfunction, sepsis-like illness, meningoencephalitis, myocarditis, hepatitis, coagulopathy and even death. Diagnosis is confirmed through PCR and culture of bodily fluids. Supportive care is the mainstay of treatment. IVIG may be beneficial for life threatening enterovirus infections and oral neomycin may be used in severe cases to control gut flora. Isolation precautions are crucial for preventing outbreaks.
Syphilis
Congenital syphilis, caused by Treponema pallidum, is on the rise, with a 300% increase in recent years. If untreated, syphilis can cause severe multiorgan involvement in newborns, including neurologic and skeletal disabilities, therefore early identification and treatment is crucial. Early signs include a characteristic maculopapular rash, nasal discharge (snuffles), and hepatomegaly. Diagnosis is made through VDRL or RPR testing, and lumbar puncture to assess for central nervous system involvement. Treatment with penicillin G is essential, and NICU Nurses must be aware that any missed doses require restarting the entire regimen.
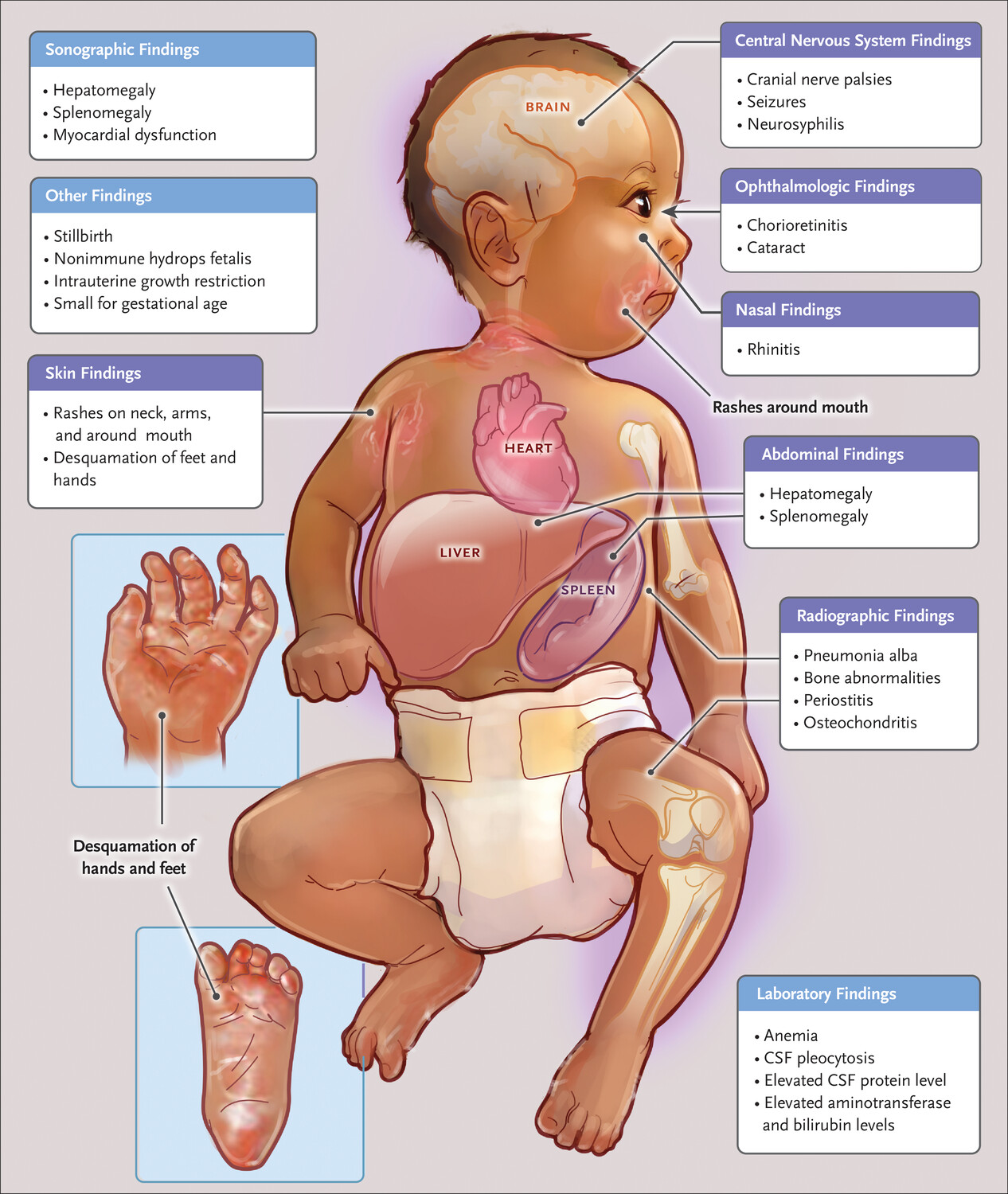
Sandoval, 2024
Varicella (Chickenpox)
Varicella, a highly communicable virus, is transmitted via direct contact with vesicular lesions or respiratory secretions. If a mother contracts varicella within 5 days before or 2 days after delivery, the newborn should receive varicella-zoster immune globulin (VZIG) to prevent severe infection. Diagnosis involves PCR of vesicular fluid, and treatment may include acyclovir and VZIG. Isolation precautions are necessary.

Ramachandra, S., Metta, A. K., Haneef, N. S., & Kodali, S. (2010)
Hepatitis B
Every year approximately 20,000 infants are born to mothers infected with Hepatitis B. Neonatal hepatitis B infection can lead to chronic hepatitis, cirrhosis, or hepatocellular carcinoma later in life. Infected infants are asymptomatic at birth but can develop chronic infection, posing significant long-term health risks. All pregnant women are screened for hepatitis B, and infants born to infected mothers are given the hepatitis B vaccine and hepatitis B immunoglobulin (HBIG) at birth. Universal immunization has reduced the incidence of acute hepatitis B infection by 98% between 1990 and 2014.
CDC Clinical Overview of Perinatal Hepatitis B
Parvovirus B19
Parvovirus B19 is not the same parvovirus that your dog may get. Sometimes referred to as “fifth disease” it is transmitted via respiratory secretions and blood and can cause fetal demise or nonimmune hydrops fetalis when a mother is infected during pregnancy. Intrauterine blood transfusion can be lifesaving to the fetus. Neonates may also present with anemia, thrombocytopenia, and the characteristic “slapped cheek” rash. Diagnosis involves testing for IgG and IgM antibodies. Intrauterine blood transfusions may be a life-saving treatment for fetuses with severe anemia.

Staroselsky, et al 2009

These congenital viral infections pose significant risks to the health of our patients, and timely diagnosis, treatment, and prevention are essential for improving outcomes. Newborns infected with congenital viral infections have long term implications including hearing loss, vision loss, developmental delays, and other complications. Neonatal nurses play a critical role in the early identification and management of these infections, ensuring that affected infants receive the best possible care. In addition, nurses are essential to family education as these babies require long term follow up from specialists ranging from ophthalmologists, developmental specialists, and infectious disease doctors.
Missed my other newsletters? Click here to read them!
Let's Study Together! Join my Certification Course
Reference:
Pammi, M., Brand, C., Weisman, L. (2021) Infection in the Neonate from Merenstein & Gardner’s Handbook of Neonatal Intensive Care (9th Ed.) Elsevier
Rudd, K. (2021) Infectious Diseases in the neonate from Core Curriculum for Neonatal Intensive Care Nursing (6th Ed). Elsevier
Gomella, T., Eyal, F., & Baby-Mohommade (2020). Gomella’s Neonatology: Management, Procedures, On-Call Problems, Diseases and Drugs (8th Ed). McGraw-Hill
https://www.cdc.gov/toxoplasmosis/hcp/clinical-overview/index.html
https://www.cdc.gov/cytomegalovirus/congenital-infection/index.html
https://www.cdc.gov/non-polio-enterovirus/about/index.html
Mcleod, Rima & Lykins, Joseph & Noble, A. Gwendolyn & Rabiah, Peter & Swisher, Charles & Heydemann, Peter & McLone, David & Frim, David & Withers, Shawn & Alibana Clouser, Fatima & Boyer, Kenneth. (2014). Management of Congenital Toxoplasmosis. Current Pediatrics Reports. 2. 166-194. 10.1007/s40124-014-0055-7.
New England Journal of Medicine (2021) Image Challenge Retrieved from https://www.nejm.org/image-challenge?ci=20211202
Sánchez Pujol, M. J., Docampo Simon, A., Sanguino, L., Blanes, M., & Betlloch, I. (2022). Herpes Simplex Virus Infection in Neonates Born to Asymptomatic Mothers: A Case Series. Cureus, 14(12), e32393. https://doi.org/10.7759/cureus.32393
Sandoval C. (2024). Syphilis Complicating Pregnancy and Congenital Syphilis. The New England journal of medicine, 390(13), 1251. https://doi.org/10.1056/NEJMc2401932
Ramachandra, S., Metta, A. K., Haneef, N. S., & Kodali, S. (2010). Fetal varicella syndrome. Indian journal of dermatology, venereology and leprology, 76(6), 724. https://doi.org/10.4103/0378-6323.72475
Staroselsky, Arthur & Klieger, Chagit & Garcia-Bournissen, Facundo & Koren, Gideon. (2009). Exposure to fifth disease in pregnancy. Canadian family physician Médecin de famille canadien. 55. 1195-8.

December 2023 Certification Review Webinar
NICU Certification Review


Ready to kickstart your journey to becoming a certified NICU nurse?
Look no further!
Grab my FREE E-Book packed with essential study and test-taking strategies for the RNC-NIC.
In the E-Book I give you the resources you need including the link to access the candidate guide, several types of books to study from, some of my favorite strategies, an outline of the content you should review, and a blank calendar for you to make your study plan!
Frequently Asked Questions About the RNC-NIC exam

What is the RNC-NIC?
The RNC-NIC is a competency-based exam that tests the specialty knowledge of nurses in the United States & Canada who care for critically ill newborns and their families.
The RNC-NICU is a nationally recognized certification that recognizes the registered nurse for their specialty knowledge and skill.

Who can take the RNC-NIC exam?
Nurses can take this exam after a minimum of two years experience in the NICU caring for critically ill newborns and their families.

Which books should I use?
I'm glad you asked! There are many excellent books to help you prepare for the RNC-NIC, I gathered ande describe each of them for you in my FREE e-book.
Is there a course to help me study?
Yes! Many hospitals host their own certification course and there are a few online courses. See my RNC-NIC test taking tips E Book for more information
What happens if I don't pass the exam?
If you don't pass the exam on your first try you can try again after 90 days. You will have to reapply after 90 days and pay a retest fee. There is no limit to the number of times you can take the exam (however a candidate can only sit for the exam twice per year).

Can I make more money if I take the RNC-NIC exam and get certified?
Yes! Many hospitals provide a raise or a bonus for nurses with specialty certifications. Hospitals also typically hire at a higher base salary when nurses have a certification.

Find me @amandasnicued on these channels or Email me
hey nurses don't miss out
© Copyright 2024. AmandasNICUEd. All rights reserved. | Terms & Conditions | Privacy Policy Contact: [email protected]

