
Welcome to Amanda's NICU Education




Hi! My name is Amanda. I'm a NICU nurse, Clinical Nurse Specialist, NICU Educator... basically your NICU BFF. If you want to talk NICU, I'm here for you! I love everything about NICU nursing and I'm eager to learn and share my knowledge with all my NICU friends.
I have been a NICU nurse since 2009 I am currently a Clinical Nurse Specialist in a Level IV NICU in Los Angeles.
I am passionate about educating the next generation of NICU nurses. I share my knowledge through platforms such as Instagram and Facebook and am excited to have you here on my website!
Click on the button below to sign up for my newsletter filled with NICU education and tips for all experience levels.

Not very many people love taking tests but as a self-acclaimed "forever student" who has taken (and passed) five different certification exams I am no longer afraid of tests! "Way to brag", you might be thinking but I want to help YOU pass your certification exam too!
Introducing Amanda's RNC-NIC Success digital course - your ultimate study companion!
Gain unlimited, on-demand access for life, ensuring you're primed to ace your certification exam.
I'm here to help you succeed and I can't wait for you to share with me that you PASSED the RNC-NIC EXAM!!!









Modes of Ventilation in the NICU

Modes of Ventilation in the NICU
In the neonatal intensive care unit (NICU), respiratory support plays a crucial role in managing the respiratory distress of fragile infants. Understanding the different modes of ventilation is essential for NICU nurses to provide optimal care. In this discussion, we will explore both invasive and non-invasive ventilation modes that are commonly used in the NICU. By familiarizing ourselves with these modes, we can enhance our knowledge and skills to effectively support newborns requiring respiratory assistance.
I. Invasive Ventilation:
Invasive ventilation involves the use of endotracheal intubation and a mechanical ventilator. The following modes are commonly seen in the NICU:
1. High-Frequency Oscillatory Ventilation (HFOV):
HFOV delivers small, rapid breaths at superimposed high-frequency oscillations. It is used in cases of severe respiratory failure or when conventional ventilation fails to provide adequate gas exchange. HFOV provides lung recruitment and optimization of oxygenation while minimizing the risk of lung injury. HFOV provides active inhalation and exhalation at a very fast rate.
2. High-Frequency Jet Ventilation (HFJV):
HFJV utilizes small, rapid bursts of gas with very low tidal volumes through a jet catheter. It is particularly useful for infants with air leak syndromes, as it allows for effective ventilation with low mean airway pressures. HFJV can help maintain lung recruitment and gas exchange in critically ill neonates. HFJV provides an active inhalation and a passive exhalation.
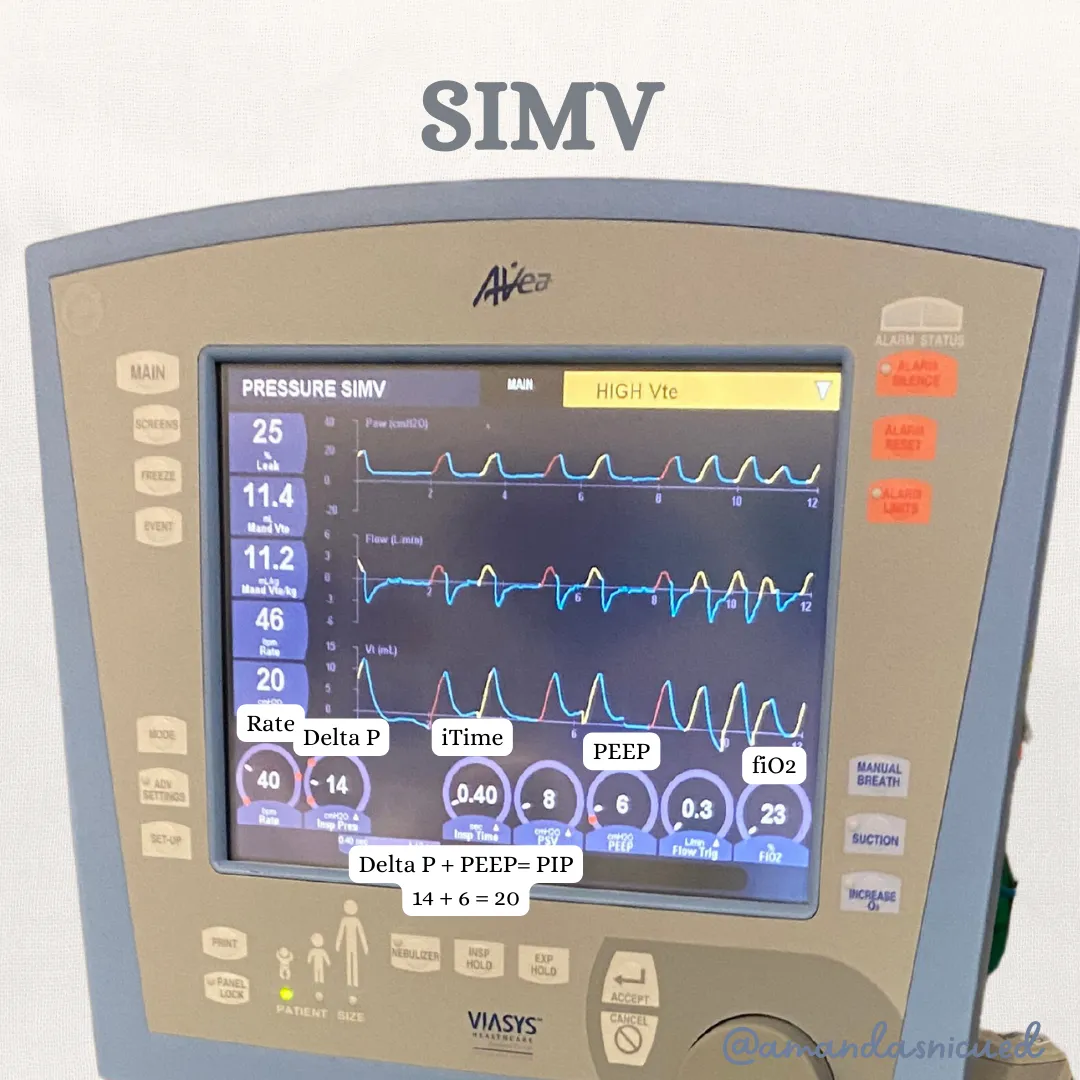
3. Synchronized Intermittent Mandatory Ventilation (SIMV):
SIMV delivers a preset number of mandatory breaths per minute, synchronized with the infant's spontaneous breaths. It allows the baby to have some control over their respiratory efforts while receiving support. SIMV is often used during weaning from mechanical ventilation, gradually decreasing the support provided.
4. Assist-Control Ventilation (A/C):
A/C ventilation delivers a predetermined number of mandatory breaths, but unlike SIMV, it does not synchronize with the infant's spontaneous breaths. With A/C ventilation, each breath is fully supported by the ventilator. It is commonly used in situations where the infant requires full respiratory support.
II. Non-Invasive Ventilation:
Non-invasive ventilation provides respiratory support without the need for endotracheal intubation. The following modes are frequently utilized in the NICU:
1. Nasal Intermittent Positive Pressure Ventilation (NIPPV):
NIPPV delivers positive pressure breaths via nasal prongs or a nasal mask. It helps improve oxygenation and ventilation without an endotracheal tube. NIPPV is commonly used as a transition from invasive ventilation or as initial respiratory support for infants who do not require intubation.
2. Nasal Continuous Positive Airway Pressure (NCPAP):
NCPAP delivers a constant positive pressure throughout the respiratory cycle via nasal prongs or a nasal mask. It helps maintain lung recruitment, reduce work of breathing, and improve oxygenation. NCPAP is widely used for respiratory support in preterm infants with respiratory distress syndrome (RDS) or other respiratory conditions.
3. High Flow Nasal Cannula (HFNC):
HFNC delivers humidified and heated oxygen at a high flow rate through nasal prongs. It provides a comfortable and well-tolerated form of respiratory support, improving oxygenation and reducing respiratory effort. HFNC is effective in managing mild to moderate respiratory distress and is increasingly used as an alternative to NCPAP.
4. Low Flow Nasal Cannula:
Low Flow Nasal Cannula delivers oxygen at a low flow rate through nasal prongs. While not a ventilation mode per se, it is worth mentioning as it is commonly used to deliver supplemental oxygen to stable infants who require minimal respiratory support.
Conclusion
Understanding the various modes of ventilation in the NICU is essential for NICU nurses. By familiarizing ourselves with both invasive and non-invasive ventilation modes, we can tailor respiratory support to the specific needs of each newborn. Collaboration between healthcare providers, ongoing assessment, and vigilant monitoring are key to optimizing respiratory care and promoting positive outcomes for these fragile infants.
Reference:
Kieran EA, Walsh MC. Noninvasive and invasive respiratory support. In: Cloherty JP, Eichenwald EC, Stark AR, eds. Manual of Neonatal Care. 8th ed. Philadelphia, PA: Wolters Kluwer; 2020:226-257.
Lampland AL, Plumm B, Meyers PA, Worwa CT, Mammel MC. Noninvasive pressure support ventilation in the preterm neonate: reducing endotracheal intubation, bronchopulmonary dysplasia, and ventilator-associated pneumonia. J Perinatol. 2017;37(11):1250-1255. doi:10.1038/jp.2017.117

December 2023 Certification Review Webinar
NICU Certification Review



Ready to kickstart your journey to becoming a certified NICU nurse?
Look no further!
Grab my FREE E-Book packed with essential study and test-taking strategies for the RNC-NIC.
In the E-Book I give you the resources you need including the link to access the candidate guide, several types of books to study from, some of my favorite strategies, an outline of the content you should review, and a blank calendar for you to make your study plan!
Frequently Asked Questions About the RNC-NIC exam

What is the RNC-NIC?
The RNC-NIC is a competency-based exam that tests the specialty knowledge of nurses in the United States & Canada who care for critically ill newborns and their families.
The RNC-NICU is a nationally recognized certification that recognizes the registered nurse for their specialty knowledge and skill.

Who can take the RNC-NIC exam?
Nurses can take this exam after a minimum of two years experience in the NICU caring for critically ill newborns and their families.

Which books should I use?
I'm glad you asked! There are many excellent books to help you prepare for the RNC-NIC, I gathered ande describe each of them for you in my FREE e-book.
Is there a course to help me study?
Yes! Many hospitals host their own certification course and there are a few online courses. See my RNC-NIC test taking tips E Book for more information
What happens if I don't pass the exam?
If you don't pass the exam on your first try you can try again after 90 days. You will have to reapply after 90 days and pay a retest fee. There is no limit to the number of times you can take the exam (however a candidate can only sit for the exam twice per year).

Can I make more money if I take the RNC-NIC exam and get certified?
Yes! Many hospitals provide a raise or a bonus for nurses with specialty certifications. Hospitals also typically hire at a higher base salary when nurses have a certification.

Find me @amandasnicued on these channels or Email me
hey nurses don't miss out
© Copyright 2024. AmandasNICUEd. All rights reserved. | Terms & Conditions | Privacy Policy Contact: [email protected]
