
Welcome to Amanda's NICU Education




Hi! My name is Amanda. I'm a NICU nurse, Clinical Nurse Specialist, NICU Educator... basically your NICU BFF. If you want to talk NICU, I'm here for you! I love everything about NICU nursing and I'm eager to learn and share my knowledge with all my NICU friends.
I have been a NICU nurse since 2009 I am currently a Clinical Nurse Specialist in a Level IV NICU in Los Angeles.
I am passionate about educating the next generation of NICU nurses. I share my knowledge through platforms such as Instagram and Facebook and am excited to have you here on my website!
Click on the button below to sign up for my newsletter filled with NICU education and tips for all experience levels.

Not very many people love taking tests but as a self-acclaimed "forever student" who has taken (and passed) five different certification exams I am no longer afraid of tests! "Way to brag", you might be thinking but I want to help YOU pass your certification exam too!
Introducing Amanda's RNC-NIC Success digital course - your ultimate study companion!
Gain unlimited, on-demand access for life, ensuring you're primed to ace your certification exam.
I'm here to help you succeed and I can't wait for you to share with me that you PASSED the RNC-NIC EXAM!!!









Respiratory Distress (part 3)
"These babies are very sensitive to stimuli which can exacerbate pulmonary vascular resistance, therefore the nurse caring for these babies must be a strong advocate."
Respiratory Disorders in the NICU: Part 3
As we reviewed earlier this month one of the most common reasons babies end up in the NICU is due to respiratory distress. Let's get back to basics and review some of the respiratory disorders that we see in the NICU.
Let's finish up the month by reviewing Persistent Pulmonary Hypertension and Pneumothorax!
Pneumothorax
There are several types of air leaks that we can see in NICU patients including Pulmonary Interstitial Emphysema, Pneumomediastinum, Pneumopericardium, and Pneumothorax.
Normally the pleural space has negative pressure which allows the lungs to fill with air on inspiration. A pneumothorax is a common air leak where air escapes the alveoli and accumulates in the pleural space. When air enters the pleural space there is a change in pressure (from negative to positive) which can collapse the lung.
Pneumothoraces can occur spontaneously or they can occur secondary to some type of trauma. When pneumos occur spontaneously the cause is either idiopathic (we don't know what caused it) or secondary to an underlying pulmonary disease process. High inspiratory pressure and unevenly distributed ventilation contribute to the development of a pneumothorax. Specifically some of the vent parameters that can contribute include a prolonged inspiratory time, a high PIP, high flow rates, and asynchrony between the baby and the ventilator. Some conditions have a higher incidence of pneumothorax due to their uneven lung compliance and alveolar overdistention. Think about the pathophysiology we discussed with meconium aspiration syndrome, for example.
When caring for a baby with a pneumothorax the signs we see will vary based on the size of the pneumo. The baby can be irritable, tachypneic, retracting, cyanotic, grunting, and nasal flaring. In a large pneumothorax you will also see cyanosis, decreased breath sounds on the affected side, tachycardia, and an increased blood pressure. If a tension pneumothorax is present, it is a medical emergency and the air must be evacuated immediately. Babies with a tension pneumothorax can have complete cardiorespiratory collapse manifested by bradycardia, hypotension, narrowed pulse pressures, and a shift of the apical pulse (away from the affected side). When a tension pneumothorax is present, it can severely compromise cardiac output and you may see cyanosis in the upper half of the body with pallor in the lower half.
When we suspect a pneumothorax a transilluminator can be used to assess for the presence of air, but be aware there can be false positives and false negatives. When a transilluminator is used to assess a pneumothorax the light is held directly against the chest and the glow of the light can be seen following the shape of the thoracic cavity. In the photo below, the image on the left shows a negative transillumination test as the light is only around the light source. The image on the right is a positive transillumination test, the glow of light fills the entire thoracic cavity. A chest X-Ray will confirm the presence of a pneumothorax, but in the presence of a tension pneumothorax the NICU team must act quickly!
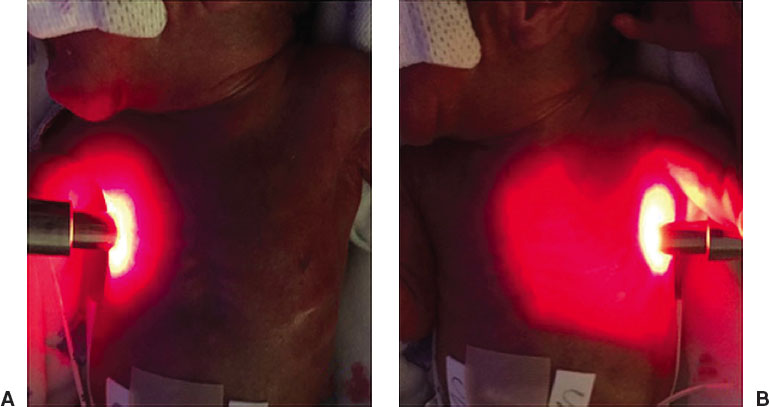
Image from Gupta A., & Dirnberger, D. (2020) Thoracostomy in Ramasethy, J. & Seo, S's Macdonal's Atlas of Procedures in Neonatology (6th Ed). Lippincott
A pneumothorax can be evacuated by a needle thoracentesis or by placing a chest tube.
A needle thoracentesis provides temporary relief while preparing for chest tube placement. When the pneumothorax is small, a thoracentesis may be all the baby needs to evacuate their air. During a needle thoracenesis an angiocatheter is inserted into the pleural space and connected to IV extension tubing, a 3-way stopcock, and a syringe. To evacuate the air, the stopcock must be turned off to atmosphere while air is aspirated into the syringe. Once the syringe is full the stopcock can be turned off to the patient and air can be emptied from the syringe into atmosphere. Those steps are repeated until vital signs stabilize (if a chest tube will be placed) or until all the air is evacuated.
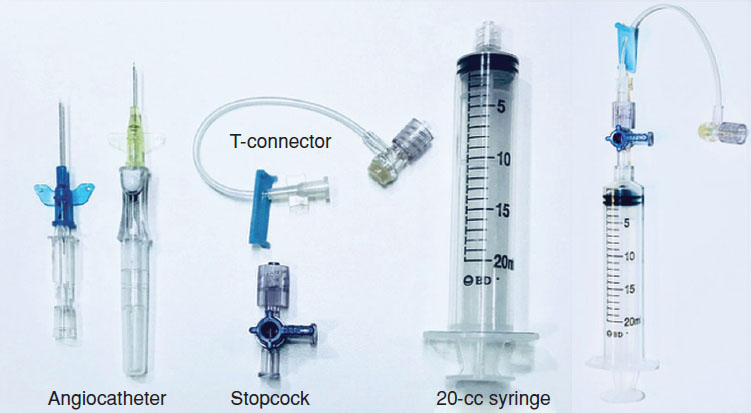
Image from Gupta A., & Dirnberger, D. (2020) Thoracostomy in Ramasethy, J. & Seo, S's Macdonal's Atlas of Procedures in Neonatology (6th Ed). Lippincott
A chest tube is an invasive procedure that can be placed via surgical incision with a straight chest tube or with a needle using a pigtail. The type and technique of chest tube insertion depends largely on experience and comfort of the provider performing the procedure.
After the chest tube is placed, it is connected to a drainage system with an underwater seal and continuous suction at 10-20cm of water. When caring for a patient with a chest tube, nurses must be familiar with the drainage device used in their NICU. There are several different types of chest tubes from single bottle systems that drain air and fluid by gravity but block atmospheric air from entering the pleural space (Heimlich valve). Additionally there are multiple bottle systems that allow suction to be applied to facilitate drainage and expansion of the lung (Pleur-Evac & Oasis). When caring for a patient with a multiple bottle system, the nurse is monitoring for bubbling in the water seal chamber. Bubbling indicates that air is being removed from the pleural space. When bubbling subsides the suction may be turned off and the chest tube is left on "water seal" meaning it is only draining by gravity. The chest tube may be removed when there has been no bubbling for at least 24 hours and no pneumothorax on chest x-ray. Chest tube removal is very painful, therefore pharmacologic and nonpharmacologic pain relief must be offered.
Pneumothorax is seen more commonly in preterm neonates and with excellent nursing and medical care these babies can recover.
Check out my IG Post on Chest Tubes
Persistent Pulmonary Hypertension
Persistent Pulmonary Hypertension (PPHN) is a condition characterized by increased pulmonary vascular resistance and vasoreactivity causing right to left shunting of blood across the foramen ovale and the ductus arteriosus (if it's patent). I find it very helpful to recall normal fetal circulation when learning about PPHN. During fetal circulation, there is high pulmonary vascular resistance (the fetus is not breathing yet) and therefore blood bypasses the lungs by shunting across the foramen ovale and the ductus arteriosus. These fetal shunts are important to normal fetal circulation.
Pulmonary hypertension can be caused by underdevelopment of the lung and its vascular bed (eg. congenital diaphragmatic hernia and pulmonary hypoplasia), it can be due to maladaptation of the pulmonary vascular bed during the transition from fetal life to neonatal life (eg. perinatal stress, hypoxia, and asphyxia), or it can be due to the maldevelopmental of the pulmonary vascular bed (eg. congenital heart defects or intrauterine asphyxia/hypoxia leading to hypertrophy of the arteries).
Another type of pulmonary hypertension we may see is chronic pulmonary hypertension associated with lung disease such as Bronchopulmonary dysplasia and Congenital Diaphragmatic Hernia. Let's focus on PPHN today
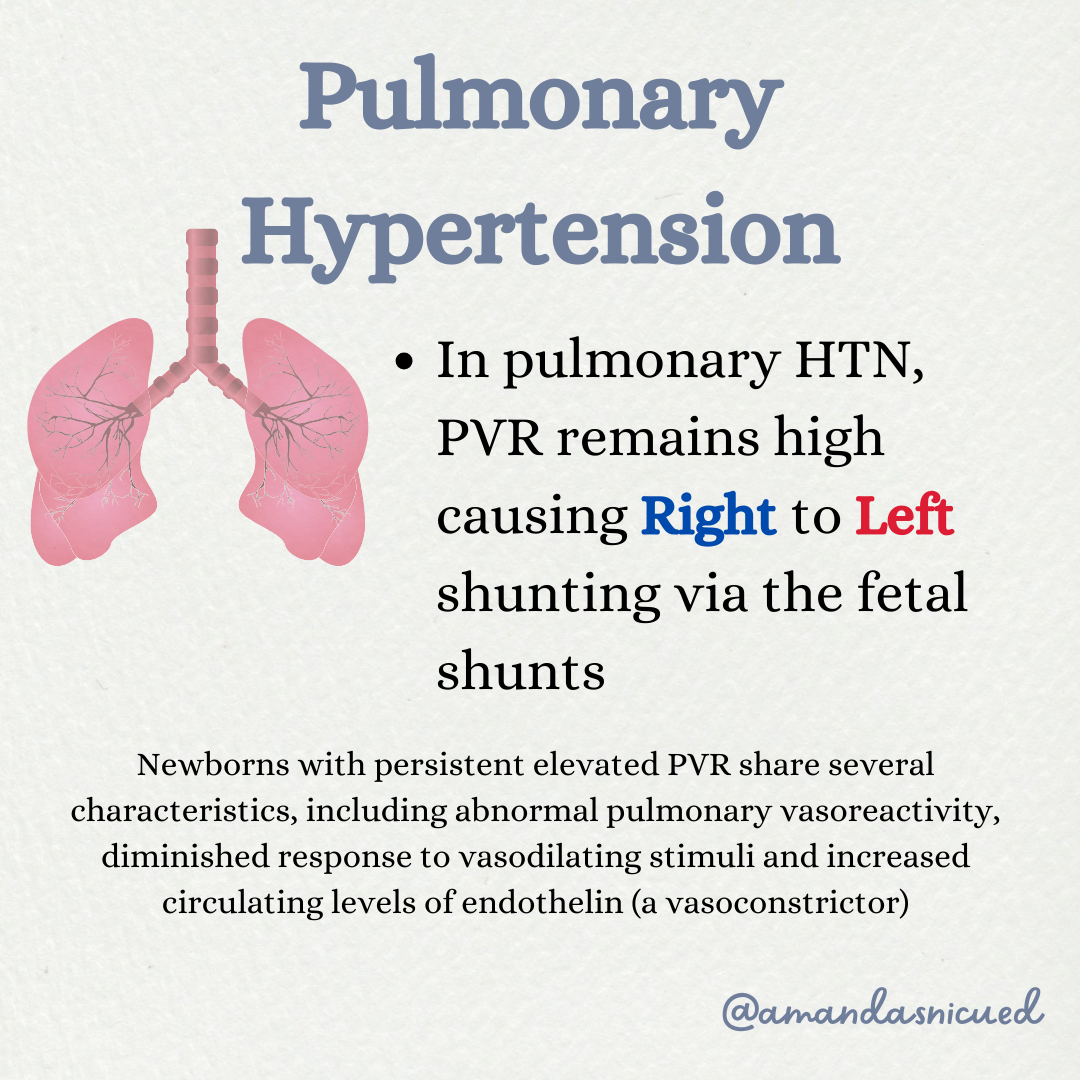
Babies with PPHN can be very sick, they have profound hypoxemia, cyanosis, acidosis, hypercarbia, and respiratory failure. We may see a difference in oxygen saturation between the pre-ductal (right upper extremity) and post-ductal saturation over 10%. This difference between pre and postductal saturation suggests right to left shunting through the fetal shunts.
Management of PPHN involves treating the associated pathology (eg. antibiotics for sepsis), improving oxygenation, reducing pulmonary vascular resistance, and increasing systemic vascular resistance to prevent right to left shunting. In some cases vasopressors will be used to maintain systemic blood pressure. Fluid management is also very important, as hypovolemia will aggravate the right to left shunt. Maintaining normal serum glucose and calcium levels are also essential as hypoglycemia and hypocalcemia can aggravate PPHN.
Sedation and analgesia are often requires to keep the infant calm and comfortable and reduce a fall in PaO2 that can be associated with routine handling.These babies are very sensitive to stimuli which can exacerbate pulmonary vascular resistance, therefore the nurse caring for these babies must be a strong advocate. Minimal handling is essential as infants with PPHN are extremely labile and has significant deterioration even with minor stimuli (noise, repositioning, or cold drafts).
Mechanical ventilation is utilized to optimize oxygenation as much as possible. Inhaled nitric oxide (iNO) may also be used to decrease pulmonary vascular resistance. The use of iNO has decreased the number of patients requiring ECMO therapy for PPHN. Sildenafil, a phosphodiesterase type 5 inhibitor, has also been successful in treating pulmonary hypertension while weaning patients off iNO.
Infants with PPHN have survival rates >70-75% with >80% of term or near term infants with PPHN expected to have essentially normal neurodevelopmental outcomes. A high incidence of sensorineural hearing loss has been seen among PPHN survivors who were treated with hyperventilation therapy (a therapy that is no longer recommended). Follow up is required for these babies after discharge. They require close cardiac supervision as pulmonary hypertension can be exacerbated during episodes of viral respiratory disease.
Let's Review Inhaled Nitric Oxide

I hope this months respiratory review was helpful! In February our focus will be on Cardiac disorders and defects 🫀
I love hearing from you, reach out to me with any questions you have or ideas for future newsletters! 😊
Wishing you all the best!
Amanda xoxo
Missed my other newsletters? Click here to read them!
Let's Study Together! Join my Certification Course
References:
Crowley, M. Neonatal Respiratory Disorders in Fanaroff, et al., Klaus & Fanaroff's Care of the High-Risk Neonate, Elsevier-Saunders, 2020
Wilson, J., & Fitzgerald, J. The Respiratory System in Jnah & Trembath's Fetal & Neonatal Physiology for the Advanced Practice Nurse. Springer 2018
Fraser, D. (2021) Respiratory Distress in Verklan, et al.'s, Core Curriculum for Neonatal Intensive Care Nursing, Elsevier.
Gardner, S., Enzman-Hines, & Nyp, M. (2021). Respiratory Diseases in Merenstein & Gardner's Handbook of Neonatal Intensive Care. Elsevier
Gomella, T, Eyal, F., Bany-Mohammed, F. (2020) Gomella's Neonatology, 8th ed., Lange

December 2023 Certification Review Webinar
NICU Certification Review


Ready to kickstart your journey to becoming a certified NICU nurse?
Look no further!
Grab my FREE E-Book packed with essential study and test-taking strategies for the RNC-NIC.
In the E-Book I give you the resources you need including the link to access the candidate guide, several types of books to study from, some of my favorite strategies, an outline of the content you should review, and a blank calendar for you to make your study plan!
Frequently Asked Questions About the RNC-NIC exam

What is the RNC-NIC?
The RNC-NIC is a competency-based exam that tests the specialty knowledge of nurses in the United States & Canada who care for critically ill newborns and their families.
The RNC-NICU is a nationally recognized certification that recognizes the registered nurse for their specialty knowledge and skill.

Who can take the RNC-NIC exam?
Nurses can take this exam after a minimum of two years experience in the NICU caring for critically ill newborns and their families.

Which books should I use?
I'm glad you asked! There are many excellent books to help you prepare for the RNC-NIC, I gathered ande describe each of them for you in my FREE e-book.
Is there a course to help me study?
Yes! Many hospitals host their own certification course and there are a few online courses. See my RNC-NIC test taking tips E Book for more information
What happens if I don't pass the exam?
If you don't pass the exam on your first try you can try again after 90 days. You will have to reapply after 90 days and pay a retest fee. There is no limit to the number of times you can take the exam (however a candidate can only sit for the exam twice per year).

Can I make more money if I take the RNC-NIC exam and get certified?
Yes! Many hospitals provide a raise or a bonus for nurses with specialty certifications. Hospitals also typically hire at a higher base salary when nurses have a certification.

Find me @amandasnicued on these channels or Email me
hey nurses don't miss out
© Copyright 2024. AmandasNICUEd. All rights reserved. | Terms & Conditions | Privacy Policy Contact: [email protected]

